Layout and Organization
ICD-10-CM is a seven-character, alphanumeric code. Each code begins with a letter, and that letter is followed by two numbers. The first three characters of ICD-10-CM are the “category.” The category describes the general type of the injury or disease. The category is followed by a decimal point and the subcategory. This is followed by up to two subclassifications, which further explain the cause, manifestation, location, severity, and type of injury or disease. The last character is the extension.
The extension describes the type of encounter this is. That is, if this is the first time a healthcare provider has seen the patient for this condition/injury/disease, it’s listed as the “initial encounter.” Every encounter after the first is listed as a “subsequent encounter.” Patient visits related to the effects of a previous injury or disease are listed with the term “sequela.”
To review: the first digit of an ICD-10-CM code is always an alpha, the second digit is always numeric, and digits three through seven may be alpha or numeric. Here’s a simplified look at ICD-10-CM’s format.
A01 – {Disease}
- A01.0 {Disease] of the lungs
- A01.01 … simple
- A01.02 … complex
- A01.020 … affecting the trachea
- A01.021 … affecting the cardiopulmonary system
- A01.021A … initial encounter
- A01.021D … subsequent encounter
- A01.021S … sequela
The ICD-10-CM code manual is divided into three volumes. Volume I is the tabular index. Volume II is, again, the alphabetic index. Volume III lists procedure codes that are only used by hospitals. (We won’t be covering ICD-10-CM Volume III codes in these courses).
ICD-10-CM is divided into ranges based on the type of injury or disease they document. For a breakdown of the ICD-10-CM coding manual download our ebook.
| Range | Topic |
|---|---|
| A00-B99 | Certain infections and parasitic diseases |
| C00-D49 | Neoplasms |
| D50-D89 | Diseases of the blood and blood-forming organs and certain disorders involving the immune mechanism |
| E00-E89 | Endocrine, nutritional and metabolic diseases |
| F01-F99 | Mental, Behavioral and Neurodevelopmental disorders |
| G00-G99 | Diseases of the nervous system |
| H00-H59 | Diseases of the eye and adnexa |
| H60-H95 | Diseases of the ear and mastoid process |
| I00-I99 | Diseases of the circulatory system |
| J00-J99 | Diseases of the respiratory system |
| K00-K95 | Diseases of the digestive system |
| L00-L99 | Diseases of the skin and subcutaneous tissue |
| M00-M99 | Diseases of the musculoskeletal system and connective tissue |
| N00-N99 | Diseases of the genitourinary system |
| O00- O9A | Pregnancy, childbirth, and puerperium |
| P00-P96 | Certain conditions originating in the perinatal period |
| Q00-Q99 | Congenital malformations, deformations and chromosomal abnormalities |
| R00-R99 | Symptoms, signs, and abnormal clinical laboratory findings, not elsewhere classified |
| S00-T88 | Injury, poisoning, and certain other consequences of external causes |
| V00-Y99 | External causes of morbidity |
| Z00-Z99 | Factors influencing health status and contact with health services |
Below, we’ve provided an example to show the levels of detail to which ICD-10 codes can go.
| ICD-10-CM |
|---|
| Injury: Closed fracture of distal phalanx of right index finger |
S00-T88 – Injury, poisoning and certain other consequences of external causesS60-S69 – Injuries to the wrist, hand and fingers
|
As you can clearly see, ICD-10-CM allows coders to code to a high level of specificity. ICD-10-CM also documents laterality—which side the injury or infection is on—and substantially increases the amount of information about the diagnosis.
Conventions
Aside from its format and organization, ICD-10-CM makes use of a number of conventions that help guide the coder to correct diagnosis codes. Some of these conventions include:
- Brackets [ ]
- Parentheses ( )
- “Includes”
- “Excludes”
- There is a slight variation here: ICD-10-CM includes two types of “Excludes” conventions
- Excludes1: lists codes that should never be coded with the code listed above. You can think of this as a “hard excludes.”
- Excludes2: lists other codes for conditions/injuries that may be a part of the condition, but are not included here. This is more of a “soft excludes.” An Excludes2 note functions similarly to a “See Also” note
- There is a slight variation here: ICD-10-CM includes two types of “Excludes” conventions
- “Code first”
- “Use Additional Code”
- “In Disease Elsewhere Classified”
- “See”
- “See Also”
- “Not Elsewhere Classified”
- “Not Otherwise Specified”
ICD-10-CM’s Excludes notes have been divided into two ‘levels.’ Excludes1 informs coders that the codes listed in the note may not, in any circumstance, be listed with the code that contains the Excludes1 note. For example, you might find something that looks like this:
- A12 {Disease} A
- Excludes1
- {disease} B, {disease} C
- Excludes1
The conditions listed in an Excludes1 note are mutually exclusive with the main condition the coder is looking up. An Excludes1 note informs the coder that if the code they are looking up is in the Excludes1 note, the coder cannot, under any circumstances, use the code that houses the note. That is, if a medical coder is looking for {disease} B, but thinks the code for {disease} A would be appropriate, the Excludes1 note would direct her to look elsewhere besides {disease} A.
Excludes2 is the other Excludes note. An Excludes2 note indicates that the code above the note does not include the other conditions listed below the note. Let’s take another look at our simplified example.
- A12 {Disease} D
- Excludes2
- {disease} E, {disease} F
- Excludes2
This Excludes2 note means that while Diseases E and F might be pertinent to or related to Disease D, they’re not found in the same code as Disease D. Unlike Excludes1, you can code conditions found in an Excludes2 note with the condition above the note. You can think of Excludes2 as sort of like “See Also,” while an Excludes1 note is more like a “See” note.
ICD-10-CM has another important convention that has to do with the code’s extensions. Remember, extensions typically provide information what encounter this is for the healthcare provider with the patient. These are not always included, but in the case that they are, they cannot simply be appended to the end of whatever code is attached. Extensions are only found in the seventh character of an ICD-10-CM code.
If a coder has to include an extension for an initial encounter on a code that does not have six characters, they must add placeholder characters. Coders use an ‘X’ for the placeholder digit.
If, for example, a coder needs to code an instance of poisoning by unintentional underdosing of antibiotic penicillin, the coder would use T36.0X1A. In this case, the fifth digit is empty, and so we’d use the placeholder character ‘X.’ Remember that placeholder characters are only used when an extension is necessary. Most ICD-10 codes do not include an extension for the encounter.
How to Use ICD-10-CM
The coding process begins with the analysis and abstraction of a medical report. Using their notes from the report, the coder may go straight to the tabular section or may refer to the alphabetic section to find the correct code, and then confirm it in the tabular.
Let’s take a look at an example.
Patient is 44-year-old Caucasian male. Self reported height and weight 1.8m and 80 kg. No notable medical history.
Patient presents with a red rash around the nose and labial folds. Some yellowish-reddish pimples. Patient complains of itching and flaking skin. Patient says rash emerged two months ago but then subsided. Diagnosed patient with seborrheic dermatitis and prescribed a topical antifungal medication.
In order to code this relatively straightforward visit, the coder would first abstract the information in the doctor’s report. The patient shows one very specific symptom (a rash on the face), and the doctor is able to make a positive diagnosis: seborrheic dermatitis.
The coder could look this up in the alphabetic index, or turn to the section in the tabular index for diseases of the skin or subcutaneous tissue: L00-L99. From there the coder would look for dermatitis and eczema and find L21: “seborrheic dermatitis.”
Underneath that category we’d find four subcategories. We’d select the one that best describes the condition diagnosed by the physician, which in this case would be L21.9, “Seborrheic dermatitis, unspecified.” We use “unspecified” here because the other codes for seborrheic dermatitis pertain either to infants or describe an “other” seborrheic dermatitis. In this case, “unspecified” is our best option.
Let’s look at the tree of codes for this diagnosis code.
L00-L99 – Diseases of the skin and subcutaneous tissue
- L21 – Seborrheic Dermatitis
- L21.0 – Seborrhea capitis
- L21.1 – Seborrheic infantile dermatitis
- L21.8 – Other seborrheic dermatitis
- L21.9 – Seborrheic dermatitis, unspecified
You’ll note that this ICD-10-CM code doesn’t have any subclassifications or extensions. Remember, not all codes need to go to the level of specificity that ICD-10-CM provides. In this case, the fourth digit is all that’s needed to describe the diagnosis.
Further Explorations
Let’s look at another example, this time an injury. Injuries often have extensions that document the encounter because the stage of treatment (whether it has not been treated, as in an initial encounter, or has already received treatment, as in a subsequent encounter) can greatly impact the medical necessity on a claim.
“Patient presents with bruising and a swollen nose and cheek after contact in a rugby match. Patient has not lost consciousness. Examination shows no rupture of the skin on the face. X-rays confirm a type II Le Fort fracture [a Le Fort fracture is one of three fractures of the bones in the face, including fractures the lower and mid maxillary bones and the zygomatic arch/cheek bone].”
We know right off the bat that this is an injury code, so we can start searching in the ICD-10-CM injury codes, found in S00-T88: “Injury, poisoning and certain other consequences of external causes.” From there we’d winnow our search to S00- S09, “Injuries to the head.”
Within that subfield of codes, we’d find S02, “fracture of the skull and facial bones.” We could also go about this by looking up a Le Fort fracture in the alphabetic index. As mentioned in the note above, a Le Fort fracture can be one of three fractures to the facial bones and skull. According to the medical report, we’re looking for a Type II Le Fort fracture.
Below S02, we’d find a number of subcategories, including codes for fractures of the vault and base of the skull, fractures of the nasal bones, and fractures of the orbital floor. We’re looking for a very specific type of fracture, however, one that involves the maxillary and zygoma bones of the face. Thankfully, there’s a specific subcategory for this: S02.4, “fracture of the malar, maxillary and zygoma bones.”
Once in this subcategory, we’d find a subclassification for Le Fort fractures (S02.4), and then three more subclassifications for each type of Le Fort fracture (S02.41). We’d select the code for our Type II Le Fort fracture: S02.412. Since this is the doctor’s first encounter with this injury, we’d use the initial encounter extension ‘A,’ and would end up with: S02.412A, “Le Fort type II fracture, closed, initial encounter.”
Now let’s look at the code tree to see how we got there.
S00-T88 – Injuries, poisonings and certain other consequences of external causes
- S02 – Fracture of skull and facial bones
- S02.0 – Fracture of vault of skull
- S02.1 – Fracture of base of skull
- S02.2 – Fracture of nasal bones
- …
- S02.4 – Fracture of malar, maxillary and zygoma bones
- S02.40 – Fracture of malar, maxillary and zygoma bones, unspecified
- S02.41 – Le Fort fracture
- S02.411 Le Fort I fracture
- S02.412 Le Fort II fracture
- S02.412A – … initial encounter for closed fracture
- S02.412B – … initial encounter for open fracture
- S02.412D – … subsequent encounter for fracture with routine healing
- Etc.
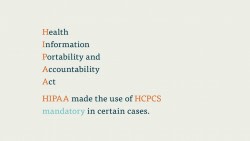
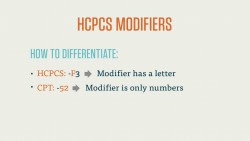
In the next few courses, we’ll introduce you to CPT codes, HCPCS codes, and their modifiers. These codes, along with the ICD codes you’ve just learned about, make up the heart of the medical coding profession.