Since medical procedures and services are often complex, we sometimes need to supply additional information when we’re coding. CPT Modifiers, like modifiers in the English language, provide additional information about the procedure. In English, a modifier may describe the who, what, how, why, or where of a situation. Similarly, a CPT modifier may describe whether multiple procedures were performed, why that procedure was necessary, where the procedure was performed on the body, how many surgeons worked on the patient, and lots of other information that may be critical to a claim’s status with the insurance payer.
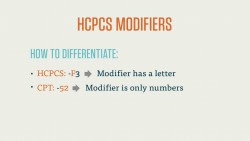
CPT Modifiers are always two characters, and may be numeric or alphanumeric. Most of the CPT modifiers you’ll see are numeric, but there are a few alphanumeric Anesthesia modifiers that we’ll look at toward the end of this course.
CPT modifiers are added to the end of a CPT code with a hyphen. In the case of more than one modifier, you code the “functional” modifier first, and the “informational” modifier second. The distinction between the two is simple: you always want to list the modifiers that most directly affect the reimbursement process first.
There’s a straightforward reason to this, too. While CMS-1500 and UB-04 forms, the two most common claim forms, have space for four modifiers, payers don’t always look at modifiers after the first two. Because of this, you always want the most important modifiers to be visible. We’ll return to this point in a few examples after we examine the CPT modifiers.
Bear in mind that each of the CPT modifiers you’ll find in this course are A) copyrighted by the American Medical Association (AMA) and B) contingent on a number of factors and guidelines. In other words, there are rules for their use. You can’t simply add a modifier to the end of a procedure code if you think it makes sense. There are, for example, a number of modifiers that state they are not compatible with Evaluation and Management (E&M) codes.
Example
Let’s take a quick look at a an example of a CPT modifier in action.
A surgeon performs a procedure to remove a bone cyst in the upper arm of a patient. The procedure also includes obtaining a graft from elsewhere in the body. Due to minor complications, the surgeon is unable to fully excise the bone cyst.
For the procedure, we’d code 23140 for “excision or curretage of bone cyst or benign tumor, humerus; with autograft (includes obtaining the graft).” Since the procedure was completed but not fully successful, we’d add the -52 modifier, for reduced services, to the code, and we’d end up with 23140-52.
Physical Status Modifier (for Anesthesia)
Anesthesia procedures have their own special set of modifiers, which are simple and correspond to the condition of the patient as the anesthesia is administered. These codes are:
- P1 – a normal, healthy patient
- P2 – a patient with mild systemic disease
- P3 – a patient with severe systemic disease
- P4 – a patient with severe systemic disease that is a constant threat to life
- P5 – a moribund patient who is not expected to survive without the operation
- P6 – a declared brain-dead patient whose organs are being removed for donor purposes
As we said, these are relatively straightforward, but let’s look at an example that will also use some of the CPT modifiers we learned just a minute ago.
Let’s return to that angioplasty example. The patient needs to be anesthetized before undergoing this procedure, so we turn to the Anesthesia section of the CPT codebook and find the code 00216 for “vascular procedures.” Now, kidney problems notwithstanding, our patient is in good health, so we’d add the –P1 modifier to this anesthesia code, and end up with 00216-P1.
Modifiers Approved for Ambulatory Surgery Center (ASC) Hospital Outpatient Use
CPT modifiers are also used in ambulatory surgery centers (ASC). These hospital outpatient facilities specialize in procedures where the patient leaves the same day.
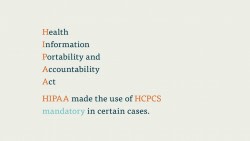
Note that there may be some overlap or contradiction with the set of HCPCS modifiers, which we’ll cover in more depth later on.
For example, HCPCS codes, which are used to report procedures to Medicare and Medicaid, have modifiers that describe which side of the body a procedure is performed on.
We won’t dive much deeper than that for now, but just know that HCPCS, another important code set that shares a lot with CPT, has its own set of modifiers, and that it’s important to note which format you need to use for a particular claim.
Supplemental Reports
Many CPT modifiers require supplemental reports to the health insurance payer. If, for instance, a payer wants to know why a surgery to repair lesions on the liver of a patient was discontinued (let’s say there was a complication with one of the proximal organs), the coder would want to file a supplementary report stating this. We both want to code to the highest level of specificity and provide as much documentation as possible. If a modifier that requires justification of medical necessity is left without a supplemental report, the claim that procedure is on may very well be rejected.